Silicosis Among Immigrant Engineered Stone (Quartz) Countertop Fabrication Workers in California
Jane C. Fazio, MD1,2,3; Sheiphali A. Gandhi, MD, MPH2,4; Jennifer Flattery, MPH2; et al
Question
What are the characteristics of patients in California with silicosis from occupational exposure to dust from engineered stone (quartz), a popular material that is high in silica content and that is used to fabricate countertops?Findings
In this case series of 52 patients, the median age was 45 years at diagnosis, and nearly all were Latino immigrant men. Diagnosis was delayed in 58%, with 38% presenting with advanced disease (progressive massive fibrosis), and 19% died.Meaning
In California, silicosis associated with occupational exposure to dust from engineered stone primarily occurred among young Latino immigrant men; many patients presented with severe disease, and some cases were fatal.Importance
Silicosis associated with inhalation of respirable crystalline silica among engineered stone countertop fabrication workers is an emerging health concern.Objective
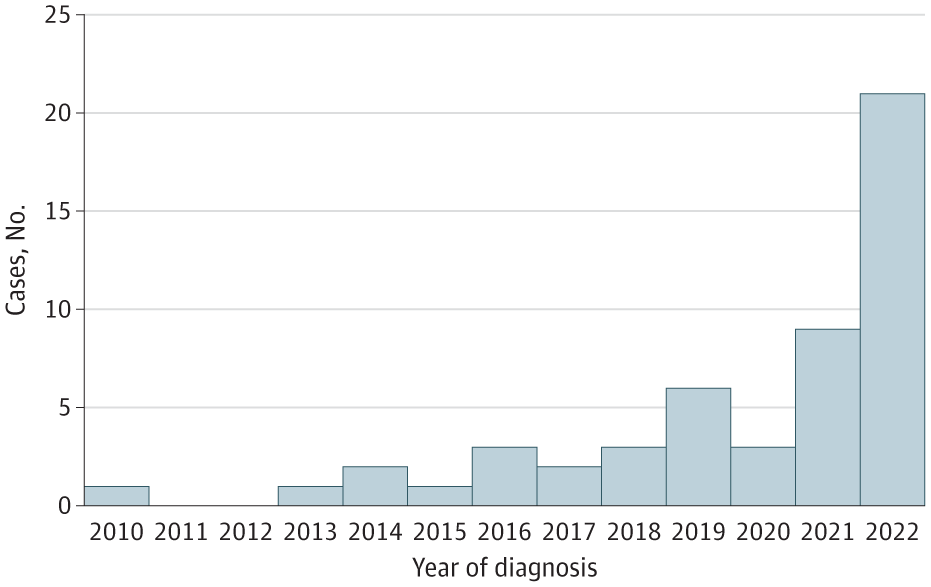
To describe clinical, socioeconomic, and occupational characteristics of patients diagnosed with silicosis associated with engineered stone in California.Design, Setting, and Participants This case series included reported cases of silicosis associated with fabrication of engineered stone countertops, as identified by statewide surveillance by the California Department of Public Health (2019-2022). Data analysis was performed from October 2022 to March 2023.
Exposures Patient interviews and medical record abstractions were used to assess occupational exposure to respirable crystalline silica, including duration of work tenure and preventive measures undertaken.
Main Outcomes and Measures
Demographics, clinical characteristics, health care utilization, and clinical outcomes were obtained, including vital status, hypoxia, and lung transplant.Results
This case series identified 52 male patients meeting inclusion criteria; median (IQR) age was 45 (40-49) years, and 51 were Latino immigrants. Ten (19%) were uninsured, and 20 (39%) had restricted-scope Medi-Cal; 25 (48%) presented initially to an emergency department. A delay in diagnosis occurred in 30 (58%) patients, most commonly due to alternative initial diagnoses of bacterial pneumonia (9 [30%]) or tuberculosis (8 [27%]). At diagnosis, 20 (38%) patients had advanced disease (progressive massive fibrosis) with severely or very severely reduced forced expiratory volume in 1 second in 8 (18%) and 5 (11%), respectively. Of the cases, 10 (19%) were fatal; median (IQR) age at death was 46 (38-51) years, and 6 patients (12%) were alive with chronic resting hypoxia. Eleven were referred for lung transplant: 3 underwent transplant with 1 fatality; 7 were declined transplant, with 6 fatalities; and 1 died prior to listing. Median (IQR) work tenure was 15 (10-20) years; 23 (45%) reported use of water suppression for dust mitigation, and 25 (48%) continued to fabricate stone after being diagnosed with silicosis.Conclusions and Relevance
In this case series performed in California, silicosis associated with occupational exposure to dust from engineered stone primarily occurred among young Latino immigrant men. Many patients presented with severe disease, and some cases were fatal.
Wet cutting, ventilation, properly fitted with masks. It’s easy to fix this issue, but it does cost money.
This is unsafe work practices rather than an issue with the stone.
Ain’t that true for so many things?
And given the scale of these operations it’s not a HUGE percentage, but you know…. Profits.
Your title reads like immigrants are more susceptible to silicosis than non-immigrants.
🤖 bleep bloop 🤖
Noted and fixed.
🤖 bleep bloop 🤖
Reminds me of back when I was in college and worked at a circuit board factory at night. Masks were not allowed and everyone made fun of me for wearing gloves. When those gloves wore out and got holes, my manager said they were “too expensive” to replace - even though management provided a bunch of PPE we were not “allowed” to use (earplugs, goggles, gloves, replacement hand tools, etc) because it would drive up the department’s budget.
I’m glad I only had to do it for four years. It’s been a decade since I quit and I STILL feel fiberglass in my hands sometimes. When I worked there my insurance basically only covered ER visits so I never used it. Now that I’m white collar I can afford to get checkups for the long term effects of that job - but most doctors seem completely untrained in caring for the consequences of manual labor.